
Your Health Magazine
4201 Northview Drive
Suite #102
Bowie, MD 20716
301-805-6805

More Weight Control, Nutrition & Exercise Articles
A Beginner’s Guide to Home Parenteral Nutrition
Key Takeaways
- HPN delivers essential nutrients intravenously, bypassing the digestive system.
- Comprehensive training and consistent support are vital for effective HPN management at home.
- Monitoring for complications and maintaining open communication with healthcare professionals maximizes patient safety and outcomes.
For individuals who cannot absorb nutrients through their digestive system, Home Parenteral Nutrition (HPN) is a life-sustaining therapy. By providing nutrients directly into the bloodstream, HPN allows patients to maintain health and quality of life when traditional nutrition is not an option. If you or a loved one is beginning the HPN journey, it’s important to understand how the process works and where to find reliable support. Discover the basics and benefits in this easy-to-follow introduction, including practical tips to help anyone new to the process navigate their care with confidence. For a deeper dive into specific processes and common questions, the Nutrishare Home TPN resource is a valuable starting point.
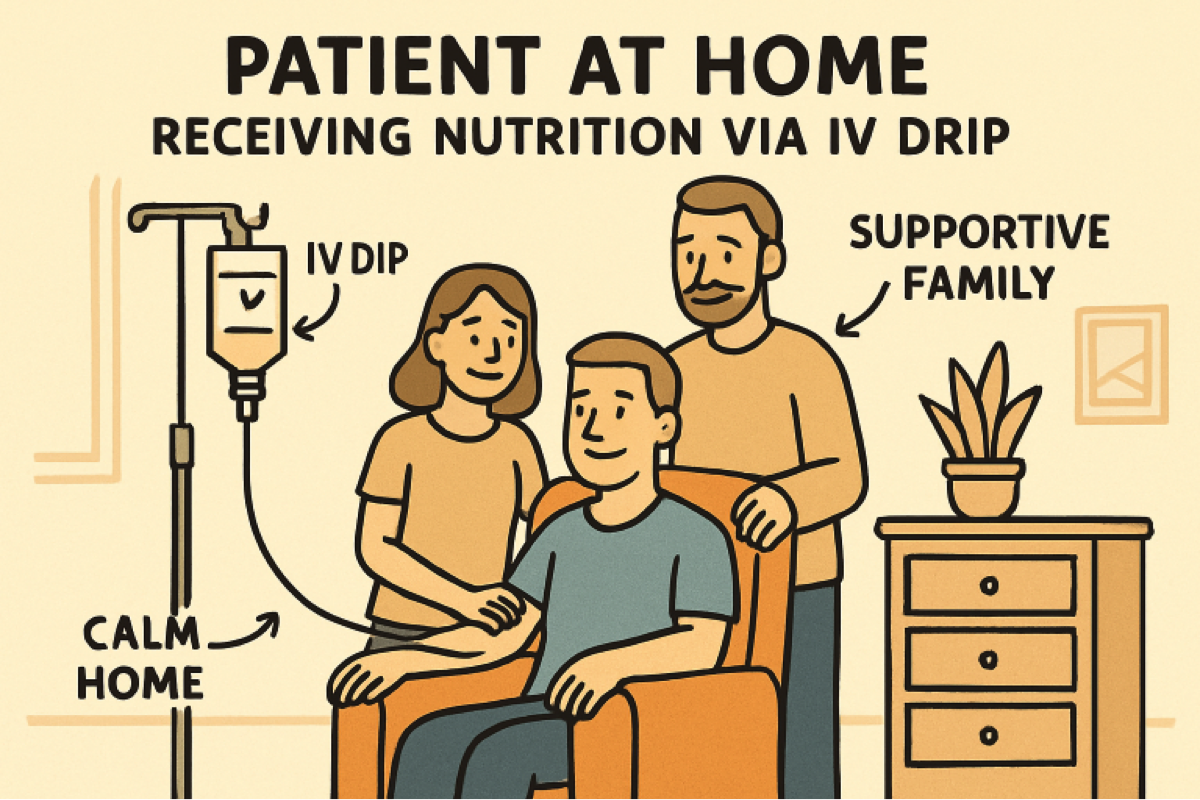
HPN brings hope and stability to many people living with chronic digestive disorders or recovering from major surgeries. The ability to manage therapy at home, surrounded by loved ones, can make a significant difference in physical and emotional well-being. Support systems, proper training, and ongoing healthcare supervision are essential in this process and will be explained throughout this guide. Whether you’re a patient, caregiver, or simply seeking knowledge, the following sections offer a clear roadmap from the basics of HPN to managing and thriving with treatment.
What Is Home Parenteral Nutrition?
Home Parenteral Nutrition (HPN) is the administration of nutrients directly into the bloodstream via a central vein, bypassing the digestive tract altogether. This highly specialized therapy is a form of Total Parenteral Nutrition (TPN). It consists of a blend of carbohydrates, proteins, lipids (fats), electrolytes, vitamins, and trace minerals tailored to the patient’s personal needs. It is most often considered when the gut is unable to process or absorb adequate nutrients to sustain life and health.
Who Needs HPN?
HPN is recommended for individuals with severe digestive conditions that render their digestive system unable to function as it should. These include:
- Short bowel syndrome often results from the surgical removal of large segments of intestine
- Crohn’s disease with severe malabsorption or complications
- Chronic intestinal pseudo-obstruction, which impairs the normal movement of food and fluids
- Intestinal obstruction that cannot be relieved surgically or medically
In these cases, even the most carefully planned diet may not meet a person’s nutritional requirements, making HPN not only beneficial but also essential for ongoing health.
Deciding on HPN requires a multidisciplinary team approach and should always be based on a thorough evaluation. According to the Mayo Clinic, the priorities include ensuring the patient’s suitability, assessing lifestyle factors, and offering clear education on potential risks and benefits.
Benefits of HPN
Home Parenteral Nutrition offers substantial benefits that extend beyond physical health. Having the flexibility to receive nutrition therapy outside the hospital can promote a sense of normalization and greater independence. Key benefits include:
- Reducing or eliminating lengthy hospital stays, allowing for home-based recovery and care
- Improving nutritional status and preventing severe malnutrition in those unable to eat normally
- Supporting participation in work, school, and recreational activities
- Providing nutritional support that is customized by your healthcare team for ongoing management and improved outcomes
For caregivers and patients alike, HPN means that day-to-day life can continue with a new sense of hope and stability. Regular monitoring ensures that therapy remains effective and adjustments are made as needs change.
Getting Started with HPN
Successfully beginning HPN at home involves coordinated planning between healthcare providers, patients, and caregivers. The key steps include:
- Comprehensive Medical Evaluation: Assessment by a multidisciplinary team including gastroenterologists, dietitians, and nurses. This includes reviewing the patient’s diagnosis, nutritional status, and daily life.
- Central Venous Catheter Placement: A special intravenous line (such as a PICC or tunneled catheter) is placed, typically in a hospital setting, to provide a reliable route for nutrient delivery week after week.
- Hands-on Training: Patients and caregivers receive targeted education on preparing, administering, and troubleshooting HPN. Training topics include sterile technique, catheter care, recognizing and responding to complications, and maintaining accurate records for daily therapy.
Training is ongoing and regularly updated to ensure the highest standard of care.
Managing HPN at Home
Day-to-day HPN management involves careful planning and adherence to hygiene protocols. Crucial steps for successful home management include:
- Following strict aseptic technique: Every step, from mixing solutions to connecting tubing and flushing the catheter, must be performed with absolute cleanliness to reduce the risk of infection.
- Monitoring for signs of complications: Patients and caregivers are educated to recognize symptoms of infection (such as redness, swelling, or fever), blood clots, or metabolic imbalances.
- Maintaining open communication: Regular check-ins with providers and dietitians ensure formulations are adjusted correctly, and questions are promptly answered. Routine blood tests and in-person or virtual appointments are a normal part of HPN management.
Support from home care agencies, combined with close coordination with pharmacists and nutrition specialists, creates a safe environment for administering therapy and addressing any challenges that may arise.
Potential Complications and How to Avoid Them
While HPN is generally safe, being aware of potential complications enables early intervention and better outcomes. Common challenges include:
- Catheter-related Infections: The most serious risk, but one that is minimized with diligent handwashing, cleaning, and dressing changes.
- Blood Clots: Presenting as swelling, pain, or changes in color in the arm, neck, or chest.
- Metabolic Imbalances: Including blood sugar abnormalities, liver dysfunction, or electrolyte shifts, which are managed by regular laboratory monitoring and close communication with dietitians and doctors.
Prompt reporting of symptoms, keeping all scheduled follow-up appointments, and thorough training all play a role in minimizing these risks and keeping therapy on track.
Final Thoughts
Home Parenteral Nutrition stands as a cornerstone therapy for patients who cannot rely on their digestive system for life-sustaining nutrition. With proper training, vigilant daily practice, and ongoing support, individuals on HPN can lead fulfilling lives while safely maintaining their nutritional needs at home.
Other Articles You May Find of Interest...
- Why Healthy Eating Doesn’t Have to Cost More (The Budget Nutrition Guide)
- How Walking for Fitness Can Turn Dangerous: Staying Safe as a Pedestrian
- Unlocking the Secrets of the Coffee Loophole Diet for Optimal Health
- Why Having Professional Guidance Accelerates Your Fitness Results
- What Causes Lower Belly Bloating? Common Triggers and When to See a Doctor
- Delicious and Nutritious Carnivore Diet Meals to Fuel Your Health Journey
- Does Effexor Cause Weight Gain? Unpacking the Truth Behind Antidepressant Effects














