
Your Health Magazine
4201 Northview Drive
Suite #102
Bowie, MD 20716
301-805-6805

More Public Safety Articles
The Ultimate Guide to Choosing the Right Toxicology Test for Accurate Results
Selecting the right toxicology test can be a crucial part of clinical care, workplace safety, legal investigations, or drug rehabilitation programs. The reliability of a toxicology report directly impacts medical decisions, treatment plans, employment screening outcomes, and legal conclusions. With multiple testing methods and specimen types available, understanding which test suits the context best helps avoid misdiagnosis, delays, or false interpretations. This guide outlines how to make informed decisions about toxicology testing, covering the key factors that influence test choice and accuracy.
Finding a Trusted Medical Testing Partner
Before choosing a test, selecting a credible diagnostic provider lays the foundation for dependable results. Accuracy doesn’t only depend on the testing method but also on the lab’s certifications, protocols, and experience. A well-established provider with a track record in toxicology will follow rigorous quality control measures and maintain transparency with clients. For example, many clinicians and organizations rely on Lynk Diagnostics as a partner that upholds these standards, offering a comprehensive range of toxicology solutions. Working with the right testing service helps avoid complications linked to errors or unclear interpretations, especially in legal or clinical scenarios where precision is critical.
Understanding the Purpose of the Test
The reason behind requesting a toxicology test shapes every aspect of the testing process—from the choice of substances included in the panel to the appropriate method and sample type. Workplace drug testing, for instance, often follows standardized guidelines set by federal or corporate policies, usually focusing on a limited panel of substances like THC, cocaine, amphetamines, opiates, and PCP. These tests are designed to identify recent substance use that may impair job performance or pose safety risks. In contrast, pain management clinics and addiction treatment centers may require more comprehensive panels that include prescription opioids, benzodiazepines, or synthetic drugs. These settings often rely on toxicology to monitor compliance with prescribed medications and detect undisclosed drug use that could interfere with treatment. Emergency departments typically prioritize speed, opting for rapid testing methods that identify substances capable of causing acute symptoms or overdose, such as fentanyl or methamphetamine. Legal cases—such as child custody disputes, probation monitoring, or accident investigations—demand highly accurate and defensible results, often confirmed through advanced techniques. Each scenario presents different expectations regarding turnaround time, sensitivity, and specificity.
Choosing the Right Sample Type

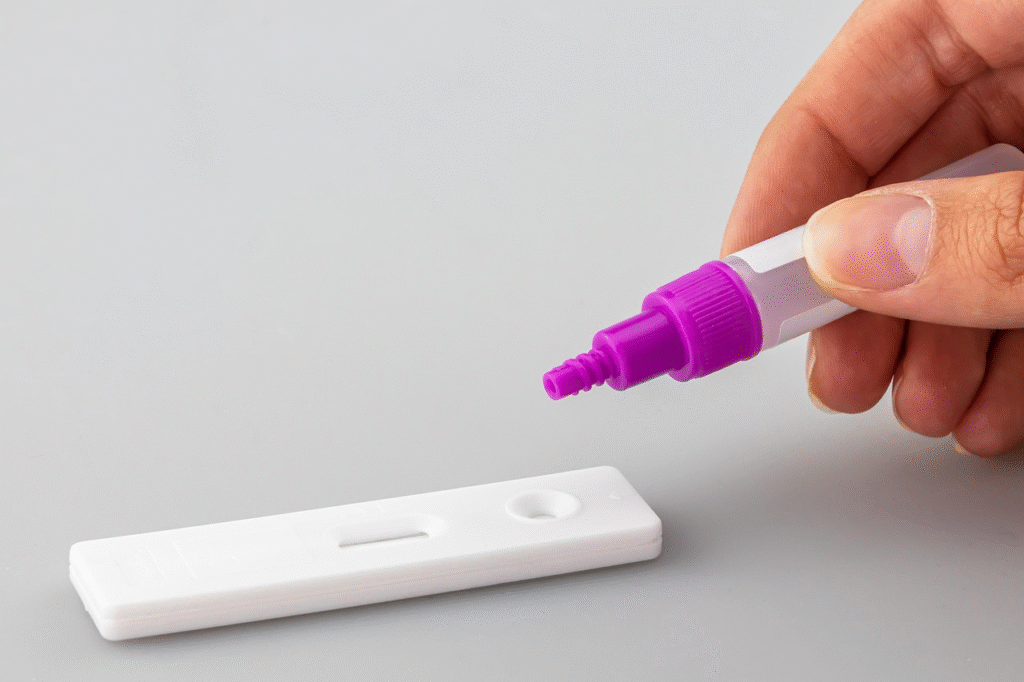
The type of biological specimen used influences what substances can be detected, how far back usage can be traced, and the invasiveness of the procedure. Urine is commonly used for its ease of collection and wide detection window for recent use. Blood tests offer insight into current impairment and are often used in clinical or forensic settings. Hair testing can reveal long-term patterns of substance use but may miss very recent exposure. Oral fluid testing provides a balance between immediacy and convenience, though it has a shorter detection window than urine. Each sample type has trade-offs, and the choice often reflects a compromise between logistical, medical, and regulatory factors.
Evaluating the Detection Window
The detection window refers to the length of time a substance remains identifiable in a biological sample after ingestion. This period varies widely depending on several factors: the type of drug, the frequency of use, the individual’s metabolism, and the sample type chosen for testing. For instance, cannabinoids like THC may be detected in hair for up to 90 days, but only for a few hours to a day in saliva. Urine tests often detect substances consumed within the last few days, making them useful for identifying recent use without being overly invasive. Blood tests, by contrast, typically reveal substances present only within the last few hours, making them well-suited for situations requiring real-time impairment data, such as roadside drug testing or emergency clinical care. Chronic or heavy use can extend the detection period of certain drugs, while occasional use may produce much shorter windows. Misunderstanding this aspect can lead to inappropriate testing choices, such as expecting a urine test to identify substance use that occurred weeks earlier. Carefully considering the detection window in light of the testing purpose is key to obtaining results that accurately reflect the timeframe of concern. A test performed too early or too late may fail to detect relevant substance use, which could lead to misleading conclusions in clinical, occupational, or forensic contexts.
Screening Versus Confirmation Testing
Initial toxicology screenings often use immunoassay techniques, which are quick and cost-effective but prone to cross-reactivity and false positives. Confirmation testing, usually performed with gas chromatography-mass spectrometry (GC-MS) or liquid chromatography-tandem mass spectrometry (LC-MS/MS), provides a more definitive result. This step is crucial when results carry significant consequences, such as employment decisions, criminal charges, or medical interventions. While screening identifies potential substances, confirmation testing quantifies them with higher accuracy. Understanding when and why to move to confirmation testing avoids misinterpretations that could have lasting impacts.
Interpreting Results with Clinical Insight
Toxicology test results require thoughtful analysis before any conclusions are drawn. A positive result can confirm the presence of a substance, but without clinical context, it may lead to misjudgment. For instance, certain medications or foods can trigger false positives on initial screenings, and metabolic variations may alter how quickly substances are eliminated from the body. A negative result, on the other hand, might occur if the test was taken outside the detection window or if the substance was not included in the panel. Misinterpretation can result in inappropriate medical treatment, wrongful employment actions, or flawed legal arguments.
Understanding test limitations and individual patient factors is just as important as the result itself. Variables like liver or kidney function, hydration levels, co-ingested substances, and genetic metabolism rates can all affect drug processing and test accuracy. Even deliberate sample tampering—such as dilution or substitution—can influence outcomes, especially in unsupervised settings. That’s why trained professionals should interpret toxicology reports within the full picture of a patient’s health history, current medications, and behavioral patterns.
Choosing the right toxicology test requires more than selecting a sample type or ticking a box on a form. It calls for alignment between the purpose of testing, the method used, and the context in which results will be evaluated. From finding a trusted diagnostics partner to interpreting results with clinical clarity, each step affects accuracy and confidence in the outcome. With informed choices, toxicology testing becomes a reliable tool across healthcare, legal, and occupational settings, serving not just to detect substances but to support decisions that matter.
Other Articles You May Find of Interest...
- Do Wasps Die After They Sting? Uncovering the Truth Behind Their Stinging Defense
- Health and Safety Best Practices for Workplaces
- The Future is Here: 5 Benefits of VR Fire Extinguisher Training
- The Right Way to Handle Sharps and Biohazard Waste
- Essential Medications: 5 Drugs You Should Never Crush for Safety and Effectiveness
- Winter Walking Safety Tips to Stay Active and Prevent Slips This Season
- How First Aid Stations Improve Workplace Safety Culture














