
Your Health Magazine
4201 Northview Drive
Suite #102
Bowie, MD 20716
301-805-6805

More Practice Management Articles
Care Coordination in Action: Integrating Behavioral Health EHR into Value-Based Care Models

What if the key to lower healthcare costs and better patient outcomes isn’t a new drug or a cutting-edge surgical procedure? What if it’s as simple — and as complex — as talking to each other?
For too long, behavioral health has been the missing piece in our healthcare puzzle. We’ve built a system that treats physical and mental conditions in separate silos, ignoring the undeniable connection between the two. The result? Higher costs, fragmented care, and frustrated patients. As value-based care demands more from us, it’s time to build a bridge between these two worlds. And the most powerful tool for that bridge? A modern, integrated behavioral health EHR.
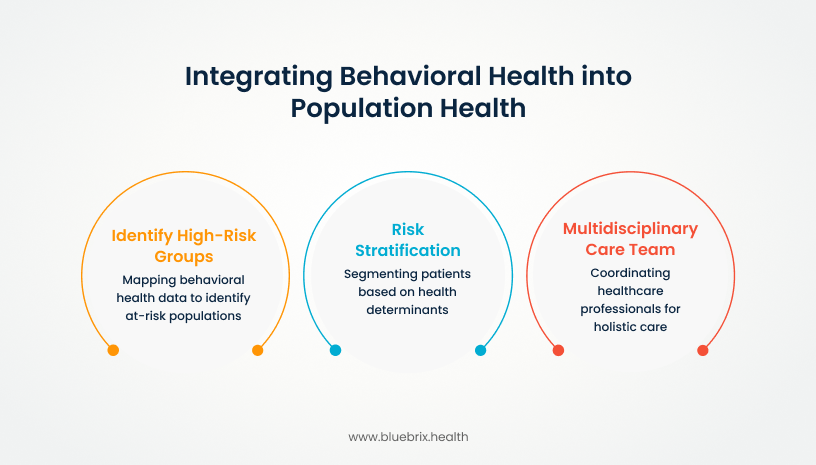
Building the Foundation: A Strategic Approach to Integration
So, how do you move from a fragmented system to a unified one? It starts with a deliberate framework. A key step is mapping behavioral health data into broader population health initiatives to identify high-risk groups. For example, a diabetic patient with comorbid depression can be flagged for additional behavioral interventions, helping to improve medication adherence and reduce complications.
This approach is deepened by risk stratification, which segments patients not just by physical diagnoses but also by behavioral and social determinants of health. This allows providers to match interventions to the populations most likely to benefit, providing more intensive coordination for those at higher risk and lighter-touch support for others.
The final piece is the multidisciplinary care team. Physicians, behavioral health specialists, care managers, and social workers all bring unique perspectives. When these caregivers are coordinated through a shared platform, they can deliver the holistic care that acknowledges both the clinical and behavioral drivers of a patient’s health.
Beyond the Basics: EHR Features that Power Integration
An EHR system built for this new reality is the engine that turns theory into practice. Here are the features that make the biggest impact:
- Shared Registries & Real-Time Alerts: These tools ensure the entire care team is instantly notified when a behavioral health crisis emerges or a medication is changed. This prevents communication gaps and allows for proactive adjustments to care plans.
- Streamlined Screening and Outcome Tracking: Tools like the PHQ-9 for depression can be built directly into the EHR workflow. This ensures consistent use and enables reliable tracking of outcomes, generating the data needed to prove that interventions are working.
- Automated Task Management & Referrals: Instead of relying on manual processes, the EHR can automatically assign follow-up tasks, trigger referral pathways, and document progress. This reduces the administrative burden on staff and ensures accountability across the team.
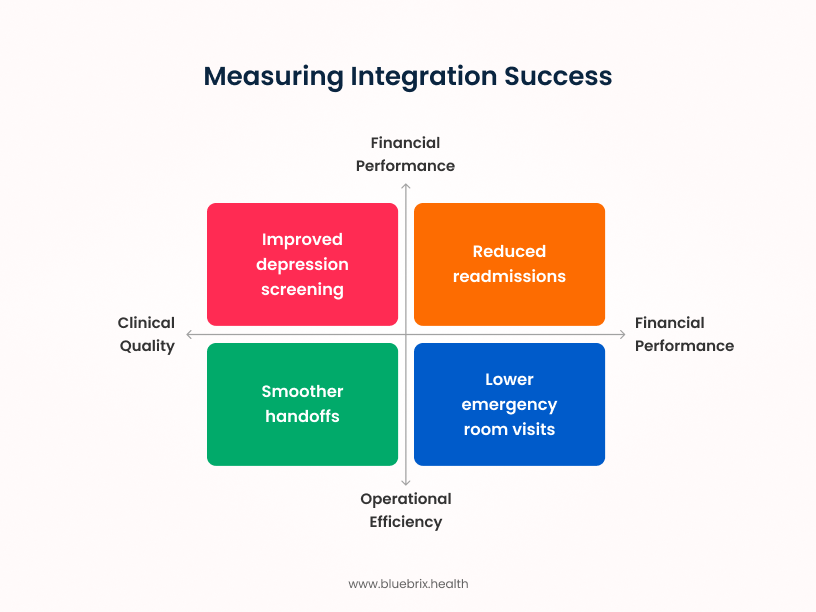
Proving the ROI: How to Measure Success
The success of integration is measured in tangible results.
- Clinical Quality: Look at key indicators like HEDIS measures for depression screening and follow-up. Consistent use of standardized tools like the PHQ-9 provides objective benchmarks for improving patient outcomes.
- Operational Efficiency: When care teams share data in real-time, duplicative testing should decline, handoffs should be smoother, and the number of patients lost to follow-up should decrease. These improvements lead to greater efficiency and higher staff and patient satisfaction.
- Financial Performance: The ultimate proof of value-based care lies in the numbers. Look for reductions in readmissions, lower emergency room visits, and decreases in the total cost of care. For Accountable Care Organizations (ACOs) and bundled-payment programs, this data is essential for both compliance and financial performance.
Your Path to Integration: A Step-by-Step Guide
Ready to get started? Here’s a practical roadmap to help you navigate the journey from fragmented care to a unified, patient-centric model.
- Pilot Planning and Cohort Selection
Instead of a big-bang rollout, start small to learn and build confidence. Identify a specific, manageable patient cohort for your pilot program. This could be patients with a high prevalence of a co-occurring condition, such as those with diabetes and depression, or a specific age group. Define clear, measurable goals for this pilot—for example, a 15% increase in PHQ-9 screenings or a 10% reduction in ED visits for the cohort. This allows your team to test workflows, fine-tune the technology, and prove the value of integration on a smaller scale before committing to a full launch.
- Clinician Engagement and Training
Technology is only as good as its adoption. If clinicians see the EHR as a new burden, your project will stall. Frame the integration not as a technology requirement, but as a tool that empowers them to provide better care and save time. Training should be hands-on and focused on workflow, not just features. Emphasize how the new system automates time-consuming tasks like referrals and documentation, freeing them up to focus on patient-centered activities. Celebrate early wins and share success stories from the pilot to build trust and demonstrate the system’s value.
- Scaling and Continuous Improvement
Once your pilot has proven its value and the team is confident in the new workflows, it’s time to scale. Gradually add broader patient populations, and expand the EHR features to include advanced analytics, automated patient outreach, or additional behavioral health tools. The work doesn’t stop once the system is live. Maintain a culture of continuous improvement through regular feedback loops, data analysis, and ongoing training. Use the data you’re collecting to identify new opportunities for care coordination and ensure the system evolves with your organization’s needs and new policy updates.
Best Practices: Lessons from the Frontlines
Organizations that have successfully integrated behavioral health have learned some crucial lessons:
- Overcoming Data Silos: Without a clean data exchange, care teams can’t function as one. Prioritize establishing interoperability standards early to prevent technical setbacks later.
- Adopting a Culture Shift: Integration is as much a cultural challenge as a technical one. Practices that frame it as a patient-centered initiative, rather than a technology project, see stronger buy-in.
- Aligning Incentives: Providers, payers, and behavioral health specialists must all see and receive value from participation. Value-based models provide the foundation for alignment, but organizations must ensure that reporting, reimbursement, and workload distribution support a truly integrated practice.
Conclusion
Integrating a purpose-built behavioral health EHR is no longer a luxury—it’s essential for delivering on the promise of coordinated, holistic care. By following a structured framework, leveraging powerful EHR features, measuring clear metrics, and embracing a deliberate implementation plan, providers can overcome the challenges and deliver measurable improvements in both outcomes and costs. The path forward is clear: behavioral health must be woven directly into the fabric of value-based care.
Want to see how an integrated EHR can transform your organization?

About the Author:
Shahzad Mohammad
Chief Product Officer at blueBriX
I’m the Co-founder and Chief Product Officer at blueBriX, where I get to combine over 16 years of HealthIT experience with my passion for building smarter, simpler solutions for healthcare teams. A big part of my focus has been on behavioural health EHRs—designing tools that actually work the way care teams do. I believe technology should reduce friction, not add to it. That’s what drives me: creating solutions that make care more connected, outcomes more measurable, and innovation easier for everyone involved.
Company: https://www.bluebrix.health/
LinkedIn Profile: https://www.linkedin.com/in/shahzad-mohammad-7646b014/
[MV1]is the repetition of financial performance intentional?
[GP2]Yes – reduced ER visits and readmissions on one side will save costs and improved screening on clinical side will also save cost.
Other Articles You May Find of Interest...
- Mind Over Marketing: Growing Your Therapy Practice
- Understanding HIPAA Standards for Healthcare Messaging: A Quick Guide for Providers
- Understanding Compliance Challenges in Protecting Patient Information
- If Your Notes Could Talk: How Smarter Clinical Documentation Protects Revenue and Reduces Audit Stress
- Top Risk Adjustment Solutions for Healthcare Providers
- A Simple Guide to Growing Your Healthcare Practice in 2026
- Certified Surgical Instrument Manufacturers Compliant with FDA Standards














