We Treat Feet and Ankles!
610 Ninth Ave
Brunswick, MD 21716
410-363-4343
1103 North Point Blvd
Suite 424
Baltimore, MD 21224
6190 Georgetown Blvd
Suite 109
Eldersburg, MD 21784
7101 Guilford Dr
Frederick, MD 21704
525 W Middle St
Gettysburg, PA 17325
372 Mill Street
Hagerstown, MD 21740
5401 Old Court Road
Randallstown, MD 21133
20 Crossroads Drive
Suite 15
Owings Mills, MD 21117
1022 Annapolis Rd, Suite B
Odenton, MD 21113
6330 Hospital Dr
Suite 104
Rosedale, MD 21237
7505 Osler Drive
Suite 503
Towson, MD 21204
826 Washington Rd
#206
Westminster, MD 21157
1160 Varnum St NE
#012
Washington, DC 20017
More Podiatry Foot Care Articles
Diabetic Foot Care
Protecting Your Feet Starts Every Day
Living with diabetes means your feet need extra attention. Not because something is wrong right now, but because the smallest change, something like a new callus, a temperature difference, or rubbing of a shoe, can quietly snowball into a serious problem. This is exactly why practices like WeTreatFeet Podiatry focus so heavily on prevention and why they work with advanced limb preservation programs to reduce amputations before they ever become a conversation. WeTreatFeet Podiatry is at the forefront of diabetic foot amputation prevention and is the only podiatry practice in Washington, DC, and the first in the region, to participate in ArcheHealthcare’s LEAP, (Lower Extremity Amputation Prevention) collaborative, a nationally recognized system designed to identify risk early and protect your limbs.
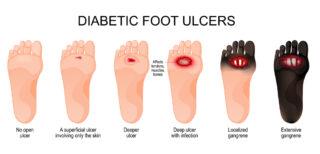
Diabetes can damage both the nerves and the blood vessels in your feet. That combination is dangerous because you can injure your foot and not even know. A small wound may not get enough blood flow to heal, and infections can spread quickly. In the worst cases, this can lead to amputation.
One subtle sign of circulation trouble is a temperature difference between your feet, for example if one foot feels noticeably cooler than the other. That is not something to brush off. It is one of the things a comprehensive diabetic foot exam is designed to pick up. When a podiatrist notices changes like this, we often order tests such as an arterial ultrasound and coordinate with a vascular specialist. The goal is not to scare you, but to catch problems early enough to treat them or slow them down.
Hammer toes and calluses may sound minor, but in a diabetic foot they can be the quiet beginning of a serious ulcer. Hammer toes bend the toes so that certain parts of the toes or the ball of the foot press harder into your shoe. That extra pressure causes rubbing and callus buildup. Under a thick callus, the skin can break down without you realizing it, especially if you have neuropathy and do not feel pain even when a deep sore is forming. This is why properly fitted diabetic shoes and custom inserts are so important. They are not just comfortable shoes. They are medical tools that spread pressure evenly across your foot, protect bony areas from rubbing, and lower your risk of ulcers and infections. For people at higher risk, podiatrists usually recommend professional nail and callus care every three to four months. Let your foot specialist handle thick nails and calluses with sterile instruments instead of trying to cut or shave them at home.
Many people with diabetes also develop onychomycosis, a fungal infection that makes the toenails thick, discolored, and crumbly. It is not attractive, and it can catch on socks or shoes, but if your circulation is compromised, aggressively removing the nail can create more danger than benefit. Removing the nail creates an open wound. Poor blood flow means that wound might not heal properly, and any open area becomes a doorway for infection, which can spread quickly in a high-risk foot. Because of that, we may recommend a conservative approach rather than nail surgery. That can include carefully thinning the nail in the office, discussing topical or oral treatments when appropriate, and focusing more on preventing pressure and trauma than on making the nail look normal. It can be frustrating to live with a nail that does not look good, but in the setting of diabetes and vascular disease, the priority is keeping the foot intact, not cosmetic perfection.
A true preventive diabetic foot exam goes far beyond a quick visual check. A thorough visit typically includes a careful skin evaluation to look for cracks, calluses, redness, blisters, or early ulcer changes, an assessment of the nails for thickness, fungal infection, or ingrowing edges, and testing of sensation with tools that check whether you can feel light touch and pressure. Temperature and circulation are assessed by comparing warmth between feet, feeling pulses, and looking at skin color and refill. Structural issues such as hammer toes, bunions, flat feet, or bone spurs can be identified because they change how you walk and where pressure lands. Practices that work within lower extremity amputation prevention programs use these exam findings in a structured way each year, so even small changes are noticed and acted on rather than missed.
No matter how advanced the clinic or technology, your daily habits are the real frontline of protection. A realistic, high risk foot care plan usually includes daily inspection of the top, bottom, and between the toes on both feet, using a mirror or help from another person if you cannot see well. You look for cuts, blisters, redness, swelling, or color changes. Daily moisturizing of the feet, avoiding the spaces between the toes, helps keep the skin from drying and cracking, which could let infection in. If you have been prescribed compression stockings, especially after a blood clot or when you have chronic swelling, using them as directed can help support the veins and control fluid buildup. Avoid walking barefoot, even at home or for a short distance, because you may not feel something sharp or hot until damage is already done. Do not perform home surgery on your feet. That means no razors on calluses, no digging at ingrown nails, and no over the counter corn removers that can chemically burn the skin.
It is also important to know your red flags and act quickly. You should contact your podiatrist or seek urgent care if you notice a new wound or blister, redness that spreads, swelling that is new or clearly worse, black, blue, or very pale areas on the skin, or a sudden change in temperature or feeling in one foot compared to the other. These signs can mean infection, loss of blood flow, or both, and they are time sensitive problems in a diabetic foot.
All of these pieces, the detailed exams, the vascular testing, the careful shoe fittings, the decision to avoid unnecessary surgery, and the time spent on education, come together with one main goal, keeping you walking on your own feet for as long as possible. That is the heart of lower extremity amputation prevention programs and a major reason it matters that WeTreatFeet Podiatry participates in this type of structured, evidence-based care. It means your visits are guided by a system specifically designed to lower your risk of ulcers and amputations, not just to treat problems once they are severe.
If you live with diabetes and have not had a comprehensive diabetic foot exam in the last year, scheduling that visit is one of the most important steps you can take to protect your mobility and independence.
Other Articles You May Find of Interest...
- Effective Remedies and Care Tips for a Broken Toe
- Effective Ways to Safely Drain Pus from an Ingrown Toenail
- Your Feet Are What You Eat
- Signs Your Toenail Fungus Is Healing: How to Know If It’s Dying
- Is Your Big Toe Numb? Discover the Causes and Solutions
- Rocker Bottom Feet: Causes, Symptoms, and Effective Management Strategies
- Is Your Iodine Level Healthy? Discover the Importance of the Iodine Test














