
Your Health Magazine
4201 Northview Drive
Suite #102
Bowie, MD 20716
301-805-6805

More Mental Health Articles
The Evolution of Ketamine Therapy: From Clinics to At-Home Treatment
The story of ketamine’s transformation from an anesthetic medication to a groundbreaking mental health treatment is one of the most remarkable developments in modern psychiatry. Even more dramatic has been the shift from expensive, clinic-based administration to accessible at-home treatment—a change that has made this potentially life-changing therapy available to millions of Americans who previously had no access.
Ketamine’s Origins: From Operating Room to Psychiatry
Ketamine was first synthesized in 1962 and approved by the FDA in 1970 as an anesthetic agent. Its safety profile and unique properties—maintaining respiration and cardiovascular function while inducing anesthesia—made it particularly valuable in emergency medicine, battlefield surgery, and pediatric procedures.
The psychiatric potential of ketamine emerged almost accidentally. Clinicians noticed that people receiving ketamine anesthesia sometimes reported mood improvements afterward. This observation sparked research into ketamine’s effects on depression, leading to groundbreaking studies in the early 2000s.
A landmark study published in 2000 by researchers at Yale and the National Institute of Mental Health demonstrated that a single low-dose ketamine infusion could rapidly reduce symptoms of depression—often within hours. This finding was revolutionary because it challenged decades of assumptions about how antidepressants work and how long they take to show effects.
The Clinic-Based Era: Pioneering but Inaccessible
Following the initial research showing ketamine’s rapid antidepressant effects, specialized ketamine clinics began opening in major metropolitan areas around 2010-2015. These facilities offered intravenous (IV) ketamine infusions, typically administered in a medical setting with people reclined in chairs for 45-60 minutes while the medication was delivered through an IV line.
The clinic model offered important advantages during this pioneering phase:
Medical Oversight: In-person medical supervision provided safety and allowed for immediate intervention if needed, which was crucial when establishing protocols for this novel use of ketamine.
Precise Dosing: IV administration offered 100% bioavailability and allowed clinicians to control dosing with precision, helping to establish optimal treatment protocols.
Controlled Environment: Clinics provided a dedicated treatment space designed to support the therapeutic experience with appropriate lighting, music, and minimal distractions.
However, the clinic-based model also created significant barriers to access:
High Costs: IV ketamine infusions typically cost $500-$1,000 per session, with a typical initial treatment course requiring 6-8 sessions. Few insurance plans covered the treatment, making it financially prohibitive for most people. The total cost for an initial treatment series often exceeded $4,000-$8,000.
Geographic Limitations: Ketamine clinics were concentrated in major cities, leaving people in rural areas and smaller communities with no access to treatment. The nearest clinic might be hundreds of miles away.
Time Requirements: Each clinic visit required not just the treatment time but also travel, waiting room time, and post-treatment observation, often consuming half a day or more per session.
Logistical Challenges: Scheduling difficulties, childcare needs, work conflicts, and transportation issues created additional barriers that prevented many people from accessing treatment even if they could afford it.
These accessibility challenges meant that ketamine therapy remained out of reach for the vast majority of Americans struggling with depression, anxiety, and PTSD—precisely the populations who might benefit most from this treatment.
The At-Home Revolution: Expanding Access Through Innovation
The development of at-home ketamine therapy represents one of the most significant advances in mental health treatment accessibility in decades. By moving treatment from clinics to people’ homes and utilizing telehealth for medical oversight, new models have made ketamine therapy available to millions of people.
Several key innovations enabled this shift:
Alternative Administration Routes: While IV administration requires clinical settings, research validated that other delivery methods could be safe and effective for at-home use. Sublingual (under the tongue) tablets and subcutaneous (under the skin) injections provided reliable absorption without requiring IV access or clinical administration.
Telehealth Integration: The expansion of telehealth platforms and regulatory changes, particularly during the COVID-19 pandemic, created pathways for remote psychiatric care. People could consult with licensed providers via video visits for assessment, prescribing, and follow-up monitoring.
Comprehensive Digital Support: Smartphone apps and digital platforms enabled people to access guided content, track symptoms, communicate with care teams, and receive integration support—all features that enhance therapeutic outcomes and safety.
Safety Protocols: Careful screening, medical monitoring systems, and clear guidelines for when in-person care is needed created safety frameworks that made home-based treatment appropriate for many people.
The impact of these innovations has been profound. At-home ketamine therapy has reduced per-session costs by approximately 60%, eliminated geographic barriers for people in many states, and allowed treatment to fit into people’s daily lives rather than requiring significant disruption for clinic visits.
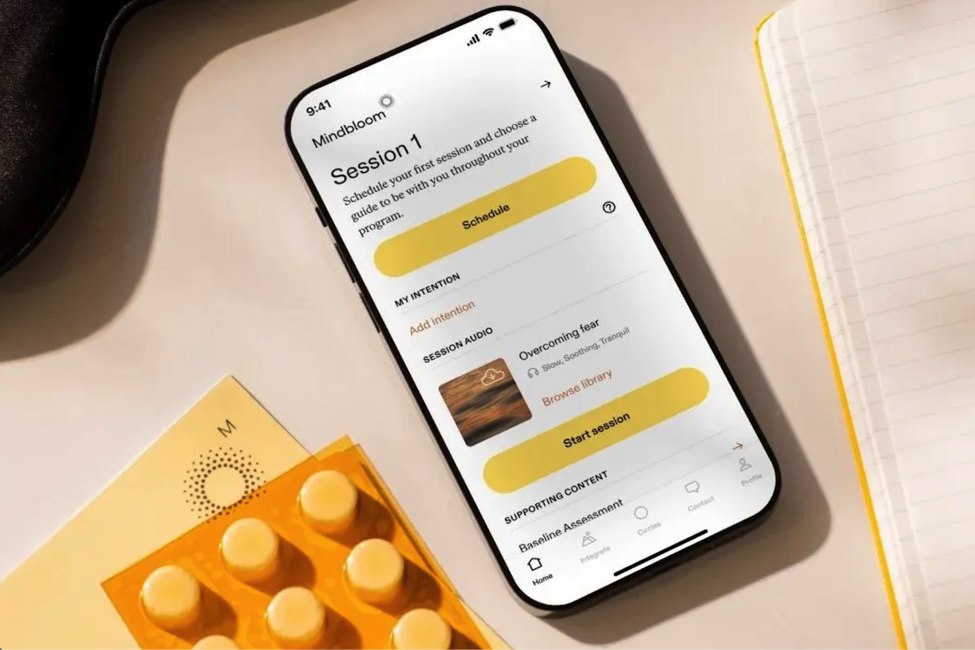
Pioneering Comprehensive At-Home Treatment
Mindbloom has emerged as a leader in making ketamine therapy accessible through its at-home treatment model. Since launching in 2019, the company has facilitated nearly 750,000 ketamine therapy sessions across 38 states, directly addressing the accessibility crisis that had previously limited ketamine treatment to a small fraction of people who needed it. By offering treatment at approximately $209 per session—compared to $500-$1,000 for clinic-based IV infusions—Mindbloom has made ketamine therapy financially feasible for a much broader population.
What makes Mindbloom’s approach particularly noteworthy is the emphasis on comprehensive care rather than medication alone. The program integrates licensed psychiatric oversight, one-on-one coaching sessions, guided therapeutic content, and community support—elements that research suggests can significantly enhance and sustain the benefits of ketamine treatment. This comprehensive model addresses a key weakness of traditional clinic-based ketamine therapy, which often provides the medication without substantial integration support or ongoing guidance between sessions. Research suggests that integration practices—what happens before and after each session—play a meaningful role in translating temporary relief into lasting change, which may help explain why Mindbloom’s outcomes exceed those seen in IV ketamine studies. The company’s outcomes, validated through the two largest peer-reviewed studies in ketamine therapy history, demonstrate that this integrated approach can be highly effective. With 89% of clients reporting symptom improvement and 28% achieving full remission from depression and anxiety symptoms, Mindbloom’s results match or exceed those reported in clinic-based studies while offering dramatically better accessibility and affordability.
For people struggling with anxiety who live in areas without access to specialized ketamine clinics, or for those who find the cost of clinic-based treatment prohibitive, programs like Mindbloom represent a meaningful alternative that doesn’t compromise on clinical oversight or therapeutic support.
Comparing Administration Methods: What the Research Shows
As ketamine therapy has evolved, different administration methods have been studied and compared. Understanding the differences can help people and providers make informed decisions about treatment approaches.
IV Infusions (Clinic-Based)
Intravenous administration delivers ketamine directly into the bloodstream, providing 100% bioavailability. The typical protocol starts with infusions at 0.5 mg/kg, though doses may be titrated up to 1.0 mg/kg or 1.2 mg/kg based on individual patient response and tolerability.
Advantages include precise dosing control and immediate medical support. However, IV treatment requires clinical settings, specialized equipment, and trained personnel for administration, contributing to high costs and access limitations. Studies have shown strong efficacy, with response rates of 40-60% in treatment-resistant depression.
Sublingual Tablets (At-Home)
Sublingual ketamine involves placing tablets under the tongue where they dissolve and are absorbed through the oral mucosa. People hold the medication in their mouth for 7-10 minutes before spitting out any remaining material.
This method offers ease of use without needles, no need for refrigeration, and flexibility in treatment timing. Research has validated sublingual ketamine as effective, with the largest peer-reviewed studies showing 89% of clients reporting symptom improvement after a series of treatments. Bioavailability is lower than IV (approximately 20-30%), but this is accounted for with adjusted dosing, and both methods have been shown to achieve comparable therapeutic outcomes.
Subcutaneous Injections (At-Home)
The newest advancement in at-home ketamine therapy involves subcutaneous injectable ketamine, which companies like Mindbloom have introduced through their injectables program. This method involves injecting the medication into fatty tissue just under the skin using small insulin-type needles. People self-administer the injection in their abdomen, and effects typically begin within 5-10 minutes.
Internal analyses of patient data have shown that injectable ketamine provides more consistent session experiences than sublingual administration, with 80% of clients reporting 5+ point improvements in depression and anxiety symptoms in preliminary real-world analyses. The bioavailability (approximately 90%) approaches that of IV administration while maintaining the convenience and cost-effectiveness of at-home treatment.
In Mindbloom’s pilot study of their injectable program, 81% of clients who had tried both sublingual tablets and injectable ketamine reported preferring the injectable format, citing consistency of effects, faster onset, and absence of taste as key factors. The injection process itself was well-tolerated, with 95% of clients successfully self-administering at home without issues. This development represents the continued evolution of at-home ketamine therapy—moving from simply replicating clinic-based treatment in home settings to innovating new delivery methods that combine the precision and consistency of clinical administration with the accessibility and comfort of at-home treatment.
The Role of Comprehensive Programs
One crucial lesson from the evolution of ketamine therapy is that medication alone isn’t enough to optimize outcomes. The most effective treatment models integrate ketamine with comprehensive support systems.
Research increasingly suggests that the therapeutic context matters significantly. Elements that enhance ketamine therapy outcomes include:
Clinical Oversight: Regular monitoring by licensed psychiatric providers who can adjust dosing, track progress, and address any concerns ensures safety and optimization of treatment.
Integration Support: Helping people process insights and experiences from ketamine sessions through structured integration practices, coaching, or therapy appears to enhance and sustain therapeutic benefits.
Guided Content: Music, meditation, breathing exercises, and other tools that support the experience during sessions can deepen therapeutic effects.
Community Connection: Access to others undergoing similar treatment can reduce isolation, normalize experiences, and provide mutual support.
Education and Preparation: Understanding what to expect, how to prepare for sessions, and how to work with the medicine enhances outcomes and reduces anxiety about the process.
Programs that incorporate these elements alongside the medication component have shown stronger outcomes in real-world settings compared to medication alone.
Evidence Base: Validating At-Home Treatment
A critical question as ketamine therapy moved from clinics to home settings was whether outcomes would remain strong. Would the convenience and accessibility come at the cost of efficacy or safety?
The evidence has been reassuring. The two largest peer-reviewed studies in ketamine therapy history, which examined outcomes from nearly 1,300 clients receiving at-home treatment, found that:
- 89% of clients reported clinically significant improvements in symptoms
- 28% achieved remission (virtually no symptoms remaining)
- 62% of clients who reported suicidal ideation at baseline no longer experienced any suicidal thoughts
- Fewer than 5% reported side effects
- Adverse events were minimal when proper screening and protocols were followed—just 0.3% reported adverse events leading them to discontinue treatment
These outcomes match or exceed those reported in clinic-based studies, suggesting that at-home treatment can be just as effective as clinic-based administration when implemented with appropriate medical oversight and support structures.
Additional research has shown that at-home treatment may offer unique advantages. Being in a familiar, comfortable environment can help people relax more fully, potentially enhancing the therapeutic effects of ketamine. The reduced cost burden also means people are more likely to complete full treatment courses rather than stopping prematurely due to financial constraints.
Addressing Safety Considerations in At-Home Settings
The safety of at-home ketamine therapy has been a primary concern as treatment has moved out of clinical settings. Extensive real-world experience has helped establish what protocols and safeguards are necessary.
Patient Screening: Comprehensive medical and psychiatric screening helps identify any contraindications before treatment begins. Conditions like uncontrolled hypertension, psychotic disorders, or current substance abuse may make at-home treatment inappropriate.
Medical Supervision: While treatment occurs at home, it remains under medical supervision through telehealth consultations, regular check-ins, and symptom monitoring. Providers can adjust treatment plans based on ongoing assessment.
Treatment Environment: People are instructed to ensure a safe space for treatment—lying down in a comfortable location, having a trusted person nearby (for initial sessions), avoiding driving or operating machinery for several hours afterward.
Emergency Protocols: Clear guidelines about when to seek emergency care and 24/7 access to clinical support provide safety nets for any unexpected situations.
Monitoring Technology: Digital symptom tracking, regular assessments, and communication platforms allow providers to monitor progress and identify any concerns between sessions.
Data from hundreds of thousands of at-home treatment sessions has shown that with these protocols in place, serious adverse events are very rare. The most common issues are mild and transient—temporary nausea, dizziness, or dissociative experiences that resolve within 1-2 hours.
Impact on Treatment of Anxiety and PTSD
While much of the initial research focused on depression, the expansion of at-home ketamine therapy has also increased access to treatment for anxiety disorders and PTSD.
Anxiety Disorders
Research published in the Journal of Psychopharmacology has shown that ketamine can reduce symptoms of generalized anxiety disorder, social anxiety, and panic disorder. The mechanism appears related to ketamine’s effects on fear conditioning and anxiety circuits in the brain.
At-home treatment has made ketamine therapy for anxiety more practical, as the treatment can be done in familiar surroundings that feel safe rather than requiring travel to clinical settings that might trigger anxiety symptoms.
Post-Traumatic Stress Disorder
Evidence suggests ketamine may help reduce PTSD symptoms through multiple mechanisms—decreasing fear responses, interrupting trauma memory reconsolidation, and promoting neuroplasticity that allows for new, adaptive neural patterns.
For trauma survivors, the ability to undergo treatment at home in a space they control can be particularly important. The sense of safety and control that a familiar environment provides may enhance therapeutic outcomes for this population.
The Economics of Access
The financial impact of moving from clinic-based to at-home treatment cannot be overstated. Consider a typical treatment course:
Clinic-Based IV Ketamine:
- 6 sessions × $750 average per session = $4,500
- Plus travel costs, time off work, childcare = Additional $500-$1,000
- Total: $5,000-$5,500 for initial treatment series
At-Home Ketamine Therapy:
- 6 sessions × $209 per session = $1,254 (as of this publication)
- No travel costs, can work around schedule
- Total: $1,254 for initial treatment series
This represents approximately 75% cost reduction, bringing treatment from economically impossible to financially feasible for many more people. For a family with a median household income, the difference between $5,000 and $1,250 can be the difference between accessing treatment or not.
Additionally, at-home treatment eliminates the hidden costs of clinic visits—lost wages from time off work, gas or public transportation, parking fees, and childcare expenses. These indirect costs often add hundreds or thousands of dollars to clinic-based treatment.
Current Landscape and Future Directions
Today’s ketamine therapy landscape is dramatically different from just five years ago. What was once available only to a small number of people in major cities has become accessible to millions across the country.
Several trends are shaping the continued evolution:
Insurance Coverage: More insurance plans are beginning to cover ketamine therapy, particularly as the evidence base grows. While coverage remains inconsistent, the trajectory is toward increased reimbursement.
Research Expansion: Ongoing studies are examining optimal dosing protocols, combination treatments with psychotherapy, predictors of response, and long-term outcomes. This expanding knowledge base will continue to refine treatment approaches.
Technology Integration: Advances in remote monitoring, digital therapeutics, and virtual reality integration may further enhance at-home treatment experiences and outcomes.
Regulatory Evolution: As at-home ketamine therapy becomes more established, regulatory frameworks are evolving to support safe, accessible treatment while maintaining appropriate oversight.
Specialized Applications: Research is exploring ketamine’s potential for other conditions including chronic pain, obsessive-compulsive disorder, and eating disorders, which could expand the scope of at-home treatment.
Making Treatment Decisions in the Current Era
For people considering ketamine therapy, the current landscape offers more options than ever before:
Clinic-Based Treatment may still be appropriate for some people who:
- Live in areas with easily accessible ketamine clinics
- Prefer in-person medical oversight during sessions
- Have medical conditions that require closer monitoring
- Have financial resources or insurance coverage that makes cost less of a concern
At-Home Treatment is increasingly the preferred option for people who:
- Live in areas without convenient access to ketamine clinics
- Need treatment to fit around work, family, or other commitments
- Are cost-sensitive and need more affordable options
- Prefer the comfort and privacy of their own space
- Want comprehensive support beyond just medication administration
The evidence suggests that both approaches can be effective when properly implemented. The “best” choice depends on individual circumstances, preferences, and resources.
A Transformed Treatment Landscape
The evolution of ketamine therapy from operating room anesthetic to clinic-based mental health treatment to accessible at-home therapy represents a remarkable arc of innovation and expanding access.
What began as a treatment available only to those who could afford expensive clinic visits in major cities has become an option for millions of Americans struggling with depression, anxiety, and PTSD. The development of safe, effective at-home treatment protocols—validated by rigorous research—has removed financial and geographic barriers that previously made ketamine therapy inaccessible for most people.
This transformation continues to unfold. As research expands, technology advances, and regulatory frameworks adapt, ketamine therapy will likely become even more integrated into mainstream mental health care. The shift to at-home treatment hasn’t just made ketamine more accessible—it’s fundamentally changed what’s possible in terms of democratizing access to innovative mental health treatments.
For the millions of people who have struggled with treatment-resistant mental health conditions, this evolution represents more than just medical progress. It represents hope—hope that effective treatment is within reach, that innovation can overcome barriers to access, and that mental health care can be both scientifically rigorous and genuinely accessible.
Other Articles You May Find of Interest...
- AI Therapy for Depression: Evidence, Benefits, and Limitations
- Law Enforcement Mental Health and Peer Support for Dispatchers: Strengthening Public Safety from Within
- Is Your Chest Tightness Linked to Anxiety? Discover the Connection
- Realistic Self-Care Rituals During the Grieving Process
- Emotional Eating: Understanding the Psychological Triggers and How to Manage Them
- How Wellness Entrepreneurs Are Using Technology to Drive Mental Health Awareness
- Mind-Body Interaction: How Stress Affects Immunity and Long-Term Health














