
Your Health Magazine
4201 Northview Drive
Suite #102
Bowie, MD 20716
301-805-6805

More Chronic Illness Articles
Understanding Lymphedema Treatment: A Guide to Products and Solutions
Receiving a lymphedema diagnosis often leaves patients with more questions than answers. This chronic condition affecting the lymphatic system requires ongoing management rather than a one-time cure.
Understanding your treatment options helps you take an active role in managing symptoms and maintaining quality of life. The good news is that modern lymphedema care has advanced significantly with better products and more effective management strategies.
This guide explains how lymphedema treatment works and what solutions are available to help you manage this condition effectively.
What Is Lymphedema?
Lymphedema occurs when lymph fluid accumulates in tissues, typically in the arms or legs. This happens when the lymphatic system cannot drain fluid properly.
The condition develops for several reasons. Primary lymphedema results from abnormalities in the lymphatic system present from birth. Secondary lymphedema develops after damage to the lymphatic system.
Cancer treatment represents the most common cause of secondary lymphedema. Surgery removing lymph nodes or radiation therapy can damage lymphatic vessels. Infection, injury or vascular conditions also trigger lymphedema development.
Symptoms typically include persistent swelling in affected limbs. The swelling may feel heavy or tight. Skin might appear stretched or thickened. Some patients experience reduced flexibility in nearby joints.
Early recognition matters significantly. Catching lymphedema in early stages allows for more effective management and better outcomes.
Core Principles of Lymphedema Management
Lymphedema requires comprehensive ongoing care rather than single treatments. Healthcare providers call this approach Complete Decongestive Therapy or CDT.
CDT combines multiple techniques addressing different aspects of the condition. Manual lymphatic drainage uses specialized massage moving fluid from swollen areas. Compression therapy applies pressure encouraging fluid drainage.
Exercise programs promote lymph flow through muscle movement. Skin care prevents infections that worsen lymphedema. Education helps patients understand their condition and management needs.
Most patients work with certified lymphedema therapists who specialize in these techniques. Initial intensive treatment typically lasts several weeks. Maintenance therapy continues long-term.
The goal isn’t eliminating lymphedema completely. Instead, treatment focuses on controlling swelling, preventing complications and maintaining function. Realistic expectations help patients stay committed to ongoing management.
Compression Therapy Fundamentals
Compression represents the cornerstone of lymphedema management. Applying external pressure to affected limbs encourages lymph fluid drainage and prevents accumulation.
Compression garments include sleeves, stockings and gloves custom-fitted to affected areas. These garments apply graduated pressure, meaning tighter compression at the extremities gradually decreasing toward the body.
Medical-grade compression differs significantly from support garments sold in drugstores. Proper lymphedema compression provides specific pressure levels measured in millimeters of mercury.
Garment selection depends on swelling severity, affected body parts and individual tolerance. Measurements must be precise for garments to work effectively without causing discomfort or circulation problems.
Most patients need daytime compression garments worn during all waking hours. Night compression options exist for patients requiring 24-hour management. Garments typically need replacement every 3-6 months as elastic fibers lose effectiveness.
Putting on compression garments takes practice and sometimes requires assistance. Donning aids like rubber gloves or special applicators make the process easier.
Advanced Treatment Technologies
Modern lymphedema care includes sophisticated devices supplementing traditional compression therapy. These technologies provide additional treatment options particularly for patients with more severe swelling.
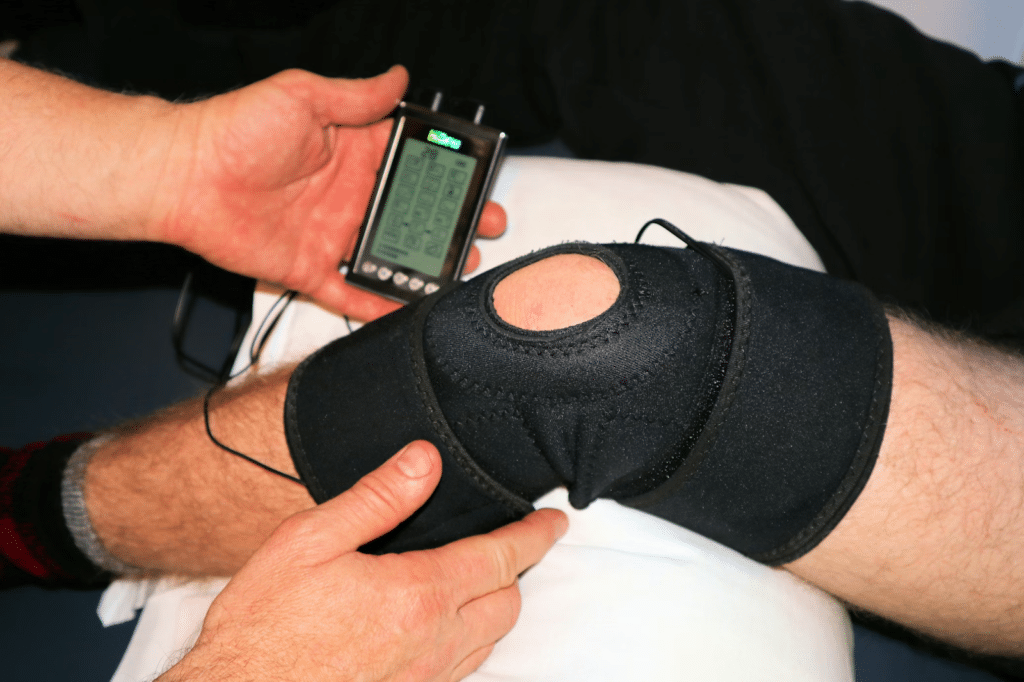
Pneumatic compression devices use inflatable sleeves connected to pumps. The pump inflates chambers in sequence, creating a massage-like effect that moves fluid from swollen areas.
Sessions typically last 30-60 minutes once or twice daily. Patients use these devices at home following physician prescriptions and training. Insurance often covers costs when devices are medically necessary.
Different systems provide various pressure patterns and intensities. Some offer simple sequential inflation. More advanced units deliver programmable pressure gradients mimicking natural lymphatic drainage patterns.

These devices particularly benefit patients with limited mobility or those unable to perform manual drainage techniques. They supplement rather than replace compression garments and other CDT components.
Understanding Available Treatment Solutions
Effective lymphedema management requires understanding what treatment solutions exist and how they work together. Modern medical technology has developed specialized lymphedema products designed specifically for comprehensive symptom control. These medical devices and therapeutic tools address various aspects of fluid management, providing patients with multiple options for both professional treatment and home care maintenance.
Treatment products fall into several categories based on their function and use. Some provide active therapy during treatment sessions. Others maintain results between active treatments. Understanding these distinctions helps patients and caregivers select appropriate solutions.
Active treatment devices typically require initial training and periodic supervision by healthcare professionals. Maintenance products like compression garments need proper fitting but patients manage them independently once trained.
Quality matters significantly with lymphedema products. Medical-grade devices undergo rigorous testing and meet specific standards. Lower-quality alternatives may prove ineffective or potentially harmful.
Insurance coverage varies by product type and medical necessity. Many insurers cover prescribed compression garments and pneumatic devices. Documentation from healthcare providers supporting medical necessity improves approval chances.
Skin Care and Infection Prevention
Healthy skin provides crucial protection against infections that worsen lymphedema. Compromised lymphatic drainage reduces immune function in affected areas, making infections more likely and serious.
Daily moisturizing prevents dry, cracked skin that allows bacterial entry. Fragrance-free, pH-balanced lotions work best. Apply after bathing while skin remains slightly damp.
Prompt wound care matters tremendously. Even minor cuts, scrapes or insect bites need immediate cleaning and monitoring. Signs of infection include increased warmth, redness, pain or fever.
Cellulitis represents the most common and serious infection complication. This bacterial skin infection can develop rapidly in lymphedema patients. Immediate medical treatment with antibiotics prevents progression.
Protection strategies reduce infection risk. Wear gloves during activities risking cuts or scrapes. Use insect repellent outdoors. Avoid tight jewelry or clothing creating skin irritation. Keep toenails trimmed carefully to prevent ingrown nails.
Exercise and Movement
Physical activity benefits lymphedema management when done appropriately. Movement stimulates lymphatic flow through muscle contraction and joint motion.
Low-impact exercises work best. Walking, swimming, yoga and tai chi provide gentle movement without excessive strain. Resistance training using light weights can help when properly supervised.
Wearing compression garments during exercise prevents swelling increases. Start gradually with short sessions. Increase duration and intensity slowly based on how your body responds.
Watch for warning signs during activity. Stop if you experience increased swelling, pain, heaviness or skin changes. These signals indicate you’ve exceeded appropriate intensity or duration.
Work with physical therapists or lymphedema specialists developing exercise programs. They provide guidance matching your fitness level and swelling severity.
Living Successfully with Lymphedema
Lymphedema requires permanent lifestyle adjustments. However, most patients achieve good symptom control maintaining active, fulfilling lives.
Consistency matters more than perfection. Following your treatment plan most days produces better results than sporadic intensive efforts. Build management activities into daily routines rather than treating them as burdensome additions.
Support systems improve adherence and outcomes. Connect with other lymphedema patients through support groups. Share experiences, practical tips and emotional encouragement. Online communities provide access when local groups aren’t available.
Stay current with your healthcare team. Regular follow-up appointments allow adjustments to treatment plans as needs change. Report new symptoms or concerns promptly rather than waiting for scheduled visits.
Advocate for yourself regarding insurance coverage, workplace accommodations and healthcare access. Understanding your rights and available resources prevents unnecessary barriers to proper care.
Moving Forward with Confidence
Lymphedema presents ongoing challenges but effective management makes tremendous difference. Understanding available treatment options empowers you to work actively with healthcare providers developing optimal care plans.
Modern compression garments, advanced devices and comprehensive therapy approaches provide better outcomes than ever before. Research continues improving products and treatment protocols.
Your active participation determines treatment success. Learn about your condition. Follow recommended management routines. Communicate openly with your healthcare team about what works and what doesn’t.
Remember that managing lymphedema is a journey rather than a destination. Expect adjustments along the way as you discover what works best for your individual situation.
With proper treatment and consistent self-care, most lymphedema patients control symptoms effectively whilst maintaining quality of life. Take advantage of available resources and don’t hesitate to seek support when you need it.
Other Articles You May Find of Interest...
- Is Your RDW Blood Test High? Understanding Its Impact on Your Health
- Empower Your Health: Essential Self-Care Strategies for Postural Orthostatic Tachycardia Syndrome
- Understanding Lymphedema Treatment: A Guide to Products and Solutions
- Navigating Life Expectancy for Those Living with Sickle Cell Anaemia
- Managing the Challenges of Nummular Psoriasis for Healthier Skin
- Stay Warm and Comfortable with Raynaud’s Disease Mittens: A Guide to Relief
- Does Barron Trump Have Marfan Syndrome and What Does It Mean for His Height?














