
Your Health Magazine
4201 Northview Drive
Suite #102
Bowie, MD 20716
301-805-6805

More Home Care & Wellness Products Articles
Weight-Loss Surgery: Options, Benefits, and Life After
Nearly 42 percent of U.S. adults live with obesity, and chances are you’ve counted calories, tried new workouts, or jumped on the latest diet—only to watch the weight return. If that cycle sounds familiar, we invite you to consider weight-loss surgery. While it isn’t the first step for everyone, the procedure can remove biological roadblocks that make traditional plans frustrating, often jump-starting steadier blood sugar, energy, and mobility. In the pages ahead, we’ll explain today’s surgical options in plain language so you can decide whether they match your health goals.
Weight loss surgery explained
Weight-loss (bariatric or metabolic) surgery changes the digestive tract so your body works with your weight-management plan. Surgeons may
- reduce the stomach to about 3–5 oz (85–140 g), helping you feel full after a few bites,
- reroute part of the small intestine to limit calorie absorption, and
- recalibrate hunger hormones such as ghrelin and GLP-1.
According to the American Society for Metabolic and Bariatric Surgery (ASMBS), patients on average lose 60–77 percent of their excess weight within 12–24 months and keep roughly half of that loss five years later. The operations are common, with about 280,000 performed in the United States in 2022, yet millions who qualify never consider them. Long-term success still relies on protein-focused meals, regular activity, and scheduled follow-up care.
Who might be a good candidate
Most programs follow long-standing NIH guidelines: adults with a body mass index (BMI) ≥ 40 kg/m², or ≥ 35 kg/m² when a serious obesity-related disease such as type 2 diabetes, obstructive sleep apnea, or hypertension is already straining health. Roughly 15 percent of U.S. adults meet these criteria, yet fewer than 1 percent proceed to surgery, according to a 2022 analysis in the National Library of Medicine.
BMI is only the first filter. A comprehensive Center of Excellence will also review your medical history, past weight-loss efforts, mental readiness, and daily support system before moving forward. The Bariatric & Metabolic Center of Colorado, a weight loss surgery institute whose patients typically lose 60 – 90 percent of their excess body weight, well above national averages, credits this multidisciplinary screening for its strong outcomes. They ask: Have you tried structured lifestyle programs? Can your heart and lungs tolerate anesthesia? Do you understand the lifelong follow-up, and do you have family or friends who can help you stay on track?
This careful vetting matches the proven benefits of surgery with people most likely to succeed while flagging any issues that could make the operation risky or the after-care unsustainable.
Types of weight-loss surgery
Bariatric programs in the United States rely on three operations that account for nearly 90 percent of all procedures: sleeve gastrectomy, Roux-en-Y gastric bypass, and duodenal switch (including its modified SADI-S form). Each reshapes the digestive tract in a different way, and their popularity reflects a balance of effectiveness, nutrition impact, and surgical complexity.
- Sleeve gastrectomy removes about 80 percent of the stomach, leaving a slender “sleeve” that holds roughly 3–5 oz (85–140 g) of food. According to ASMBS, it made up 57 percent of U.S. bariatric operations in 2022.
- Roux-en-Y gastric bypass creates a thumb-sized pouch and reroutes the small intestine in a Y-shaped loop, limiting both intake and absorption. Despite a longer learning curve for surgeons, it represented 22 percent of 2022 cases and remains the preferred choice for severe reflux or difficult diabetes, per ASMBS.
- Duodenal switch and SADI-S combine a sleeve with a more extensive intestinal bypass, producing the greatest average weight loss but requiring the most rigorous lifelong vitamin monitoring. They account for roughly 2 percent of current procedures, and referrals are rising as centers gain experience, again according to ASMBS.
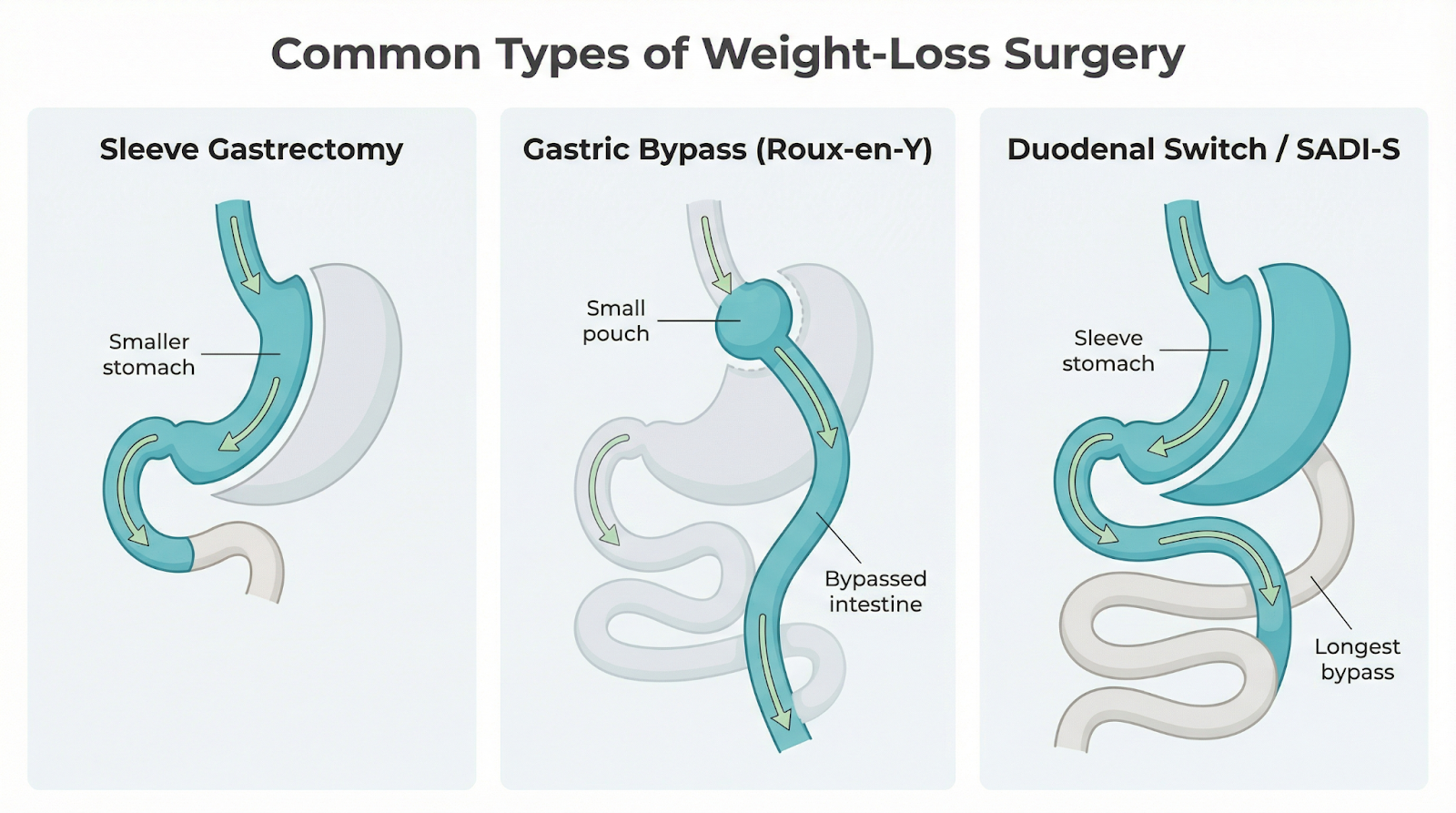
Gastric sleeve
During a laparoscopic sleeve gastrectomy, the surgeon removes about 80 percent of the stomach, leaving a slender tube that holds roughly 3–5 oz (85–140 g) of food. The smaller pouch limits portion size and sharply lowers the hunger hormone ghrelin, so you feel satisfied sooner.
A 2012 meta-analysis of more than 12,000 study participants confirms that patients lose 55–75 percent of their excess body weight in the first two years. Long-term success hinges on protein-forward meals, daily vitamin supplements, and regular check-ins with your care team.
Gastric bypass (Roux-en-Y)
Surgeons create a pouch about the size of a walnut (≈ 1 oz / 28 g) and connect it directly to the mid-small intestine, so food skips roughly 150 cm (59 in) of absorptive bowel. This tiny reservoir plus a shorter nutrient path typically leads to a 65–80 percent excess-weight loss within two years, according to multiple long-term cohort studies.
Although it accounted for a smaller share of 2022 U.S. cases (about 22 percent) than the sleeve, decades of follow-up show durable weight loss and diabetes remission in more than 80 percent of patients at five years. Lifelong vitamin supplements and yearly lab checks stay critical, because the bypassed intestine absorbs less iron, calcium, and B-vitamins.
Duodenal switch and SADI-S
A classic duodenal switch starts with a sleeve gastrectomy, then routes food around roughly three-quarters of the small intestine, leaving about 250–300 cm (8–10 ft) for absorption. The single-anastomosis version (SADI-S) shortens that bypass while keeping a strong hormonal effect. Both operations deliver the greatest average weight loss in bariatric surgery, about 75–85 percent of excess pounds at two years, and diabetes remission rates up to 90 percent, according to recent meta-analyses.
This power has a price. Without diligent supplements, more than 60 percent of patients develop vitamin A or D deficiencies by year 4, and lifelong lab monitoring stays essential. Because the operation is complex, it represented only about 2 percent of U.S. bariatric cases in 2022, but referrals are rising for people who regain weight after other surgeries.
Your surgical team balances maximum metabolic impact against rigorous follow-up care to decide whether a duodenal switch or SADI-S fits your goals and lifestyle.
Benefits and risks
Bariatric surgery is the only obesity treatment proven to deliver double-digit, long-term weight loss and often remission of weight-related diseases. Yet, like any operation, it carries downsides that warrant equal attention.
Why many patients see more upside than downside
- Weight loss that sticks. Most people lose 25–35 percent of their starting weight (about 60–70 percent of excess pounds) within 12–24 months and keep at least half of that off five years later.
- Metabolic reset. Large U.S. cohorts show 56–60 percent of patients with type 2 diabetes reach remission within a year, and roughly half maintain it at five years.
- Cardiovascular lift. Average systolic blood pressure drops 9–13 mm Hg (1.2–1.7 kPa) and HDL cholesterol rises 7–10 mg/dL within 12 months, lowering heart-disease risk.
- Better sleep and mobility. More than 70 percent of patients report that obstructive sleep apnea resolves and knee or back pain eases, making daily activities feel easier.
Risks to weigh and manage
- Low early mortality. Modern laparoscopic techniques keep the 30-day death rate near 0.1 percent, similar to gallbladder surgery; risk rises with age, very high BMI, and multiple illnesses.
- Surgical complications. Leaks or bleeding occur in roughly 1–2 percent of cases; blood clots or pulmonary embolism in 0.3–0.5 percent.
- Nutrient gaps. Without daily supplements, up to 60 percent of duodenal-switch patients and 20–30 percent of sleeve or bypass patients develop vitamin D, B12, or iron deficiencies within four years.
- Digestive adjustments. Food intolerances, dumping after sugary meals, or chronic diarrhea affect 10–30 percent of patients, depending on the procedure.
- Psychological shifts. Rapid body changes can prompt mood swings or changes in eating behavior; ongoing counseling is recommended.
We partner with you to personalize these numbers to your health profile, then build a plan that combines nutrition classes, mental-health check-ins, and lifelong labs to boost gains and keep complications uncommon.
Life after weight-loss surgery
The operation lasts a few hours; the lifestyle that follows lasts a lifetime. Studies show that patients who keep follow-up visits, take daily supplements, and stay active lose an additional 8–10 percentage points of excess weight compared with those who drop out of care.
Success rests on four habits:
1. Eat with intention. Enjoy five to six protein-first meals the size of a deck of cards, chewed thoroughly, to keep muscle strong while the pouch or sleeve heals. Sugary drinks and “slider” foods pass through the stomach quickly and often trigger regain.
2. Move most days. Even brisk ten-minute walks (about 800 m) started in week one help preserve lean mass. By three months, most programs encourage at least 150 minutes of moderate activity each week.
3. Show up for labs and check-ins. Bariatric centers schedule at least five visits in the first year and annual labs thereafter. Skipping appointments doubles the risk of vitamin D or B-12 deficiency by year four.
4. Lean on community. Whether it is an in-person class or a private online group, regular support participation links to an extra 7–9 percent excess-weight loss at two years.
Conclusion
Patients who weave these rhythms into daily life report steadier energy, fewer binge triggers, and confidence to hike, dance, or play with their children. The real transformation unfolds long after the last surgical stitch.
Other Articles You May Find of Interest...
- What Causes Knuckle Swelling and How to Alleviate It?
- Can a Leaky Roof Make You Sick?
- Managing Indoor Air During Season Changes
- Weight-Loss Surgery: Options, Benefits, and Life After
- Effective Home Remedies for Relieving Cervicogenic Headaches
- Home guide to EMF in 2025: how to measure, compare, and reduce exposure
- The DIY Bed Bug Treatment That Outsmarts Pest Control














